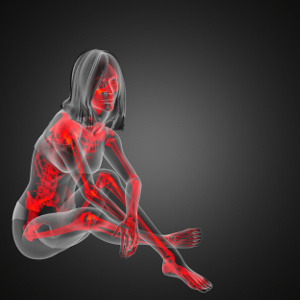
Osteoporosis is often linked to undetected lack of magnesium
 Calcium and vitamin D normally get all the attention when it comes to bone health. However, magnesium also plays a crucial, but often overlooked, role. This was demonstrated in a large population study that is published in Frontiers in Nutrition. The study links lower dietary magnesium to a greater risk of developing osteoporosis, especially for women aged 55 years and older. Osteoporosis normally takes many years to develop so it is vital to get plenty of magnesium from the diet or from supplements. Also, beware that excessive calcium intake, antacids, and diuretics block the body’s ability to absorb and utilize magnesium.
Calcium and vitamin D normally get all the attention when it comes to bone health. However, magnesium also plays a crucial, but often overlooked, role. This was demonstrated in a large population study that is published in Frontiers in Nutrition. The study links lower dietary magnesium to a greater risk of developing osteoporosis, especially for women aged 55 years and older. Osteoporosis normally takes many years to develop so it is vital to get plenty of magnesium from the diet or from supplements. Also, beware that excessive calcium intake, antacids, and diuretics block the body’s ability to absorb and utilize magnesium.
The new study aimed at investigating the relation between dietary magnesium intake and MDS (magnesium depletion score), a specific score for magnesium deficiency in adult Americans with detected osteoporosis. The researchers collected data from the large NHANES population study during the period 2005-2018. A total of 14,566 participants were included in the analysis. Several models were employed to reveal various links between dietary magnesium intake and the rate of osteoporosis. The scientists even looked at the magnesium supplements’ absorbability and bioavailability.
After adjusting for various confounders such as gender, age, BMI, and smoking, the team of scientists could see a negative correlation between dietary magnesium and osteoporosis, especially among women from 55 years and older.
The new study shows that people who consume less than the recommended amount of magnesium are more likely to develop osteoporosis. According to the study results, people who get too little dietary magnesium should ideally have a bone density test carried out to see if they have osteoporosis.
The new study also suggests increased focus on magnesium to help prevent osteoporosis.
- The bone disease that takes several years to develop can even affect younger people.
- In Denmark, around one in three women and one in eight men are affected by osteoporosis.
Osteoporosis has serious and potential life-threatening consequences
Osteoporosis is a bone disease that causes the microstructure in bone tissue to deteriorate. Also, the mineral density in the bones is low, which weakens the bones and increases the risk of a fracture. Bone fractures often impair quality of life, and many people, especially older seniors, sustain a fractured hip as a result of falling. This typically leads to complications, admission to nursing home, and death after as little as one year.
Many factors increase the risk of osteoporosis – including genetic factors, hormonal factors, lack of exercise, and unhealthy diets. It is commonly known that calcium is of vital importance to bone health, and vitamin D is important for the absorption of calcium in the body. That is why most supplements for bone health only contain these two nutrients. It’s not enough, however.
Magnesium affects bone health in several ways
In recent years, there has been increased focus on other nutrients in relation to musculoskeletal diseases, for example magnesium. This is because magnesium is an essential co-factor of enzymes related to the synthesis of the bone matrix and the bone-building cells called osteoblasts. Magnesium controls that the right amount of calcium is channeled into the bone cells where it is needed.
Magnesium deficiency affects the parathyroid glands that help control the calcium levels in the blood. Lack of magnesium can also inhibit the uptake of calcium in bone cells and the vitamin D levels in the blood, thereby impairing the mineral density of bone tissue. Magnesium deficiency can also trigger harmful inflammation and stimulate increased activity of the osteoclasts, which are cells that break down old and worn-out bone tissue.
Earlier studies have shown that low dietary magnesium intake is associated with lower bone mineral density in the hips, among other places. A meta-analysis (Farsinejad-Marj et al.) has shown that diets with sufficient magnesium are positively related with bone density in the neck and hips. Other than that, the majority of studies have focused on the amount of magnesium in the diet, but have failed to look at the body’s uptake of the nutrient. For that reason, the scientists behind the new population study used the new magnesium deficiency score (MDS) that provides a more reliable picture of the body’s uptake and excretion of magnesium. A higher MDS score means that the bioavailability of magnesium from the diet is low. That way, the MDS system gives a better understanding of the body’s magnesium status and can more easily detect a deficiency.
The scientist state that no previous studies have looked at the relation between magnesium deficiency and osteoporosis based on the MDS system. Their new study therefore paints a more accurate picture of the relation between magnesium in the diet, magnesium’s bioavailability, and the risk of developing osteoporosis.
What contains magnesium, and what impairs the body’s uptake of the nutrient?
Magnesium is mainly found in wholegrains, nuts, kernels, cabbage, beans, and other compact vegetables. Ageing, low stomach acid, elevated calcium levels, antacids, and blood pressure-lowering medication impairs the uptake of utilization of magnesium. Having too little vitamin D in the blood also has this effect. Moreover, a large intake of alcohol, insulin resistance, diabetes, diuretics, and diarrhea increase the body’s excretion of magnesium.
In Europe, the official recommendation for magnesium is 350 mg for men and 300 mg for women. Even higher levels may be required if you are magnesium-deficient or have problems with utilizing the nutrient.
References:
Associations of the Dietary Magnesium Intake and Magnesium Depletion Score With Osteoporosis Among American Adults: Data From the National Health and Nutrition Examination Survey. Jie Want, Fei Xing, Ning Sheng, Zhou Xing.
Front Nutr. 2022; 9: 883264.
Search for more information...
- Created on .








