Q10 supplements protect against chronic inflammation and oxidative stress
- and oxidative stress
 The body uses inflammation as part of its normal immune response to infections and tissue damage. If inflammation becomes chronic, however, it can be extremely dangerous. What happens is that it bombards the body with free radicals. This leads to oxidative stress and increases the risk of cell damage, overweight, and chronic diseases like type 2 diabetes, cardiovascular disease, autoimmune diseases, and different cancer forms. Diet and lifestyle play a major role, and according to a meta-analysis published in Frontiers in Pharmacology, Q10 supplementation can lower several markers of inflammation and oxidative stress.
The body uses inflammation as part of its normal immune response to infections and tissue damage. If inflammation becomes chronic, however, it can be extremely dangerous. What happens is that it bombards the body with free radicals. This leads to oxidative stress and increases the risk of cell damage, overweight, and chronic diseases like type 2 diabetes, cardiovascular disease, autoimmune diseases, and different cancer forms. Diet and lifestyle play a major role, and according to a meta-analysis published in Frontiers in Pharmacology, Q10 supplementation can lower several markers of inflammation and oxidative stress.
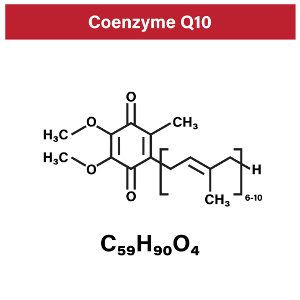
Q10 is a coenzyme that plays a role in cellular energy metabolism. It also serves as an antioxidant. The body is able to produce the compound, but our endogenous Q10 synthesis starts to decrease when we reach our twenties. Cholesterol-lowering statins and osteoporosis medication (alendronate) can also impair the body’s Q10 synthesis, and the same is the case with many diseases. Meta-analyses have shown that supplementation with Q10 has a positive effect on markers of inflammation and oxidative stress, while other studies have failed to demonstrate this. One possible explanation is that the Q10 preparations used in the trials had inferior quality, that the dosage was too low, that the study duration was too limited, or that the scientists used different analysis methods.
The researchers behind the new and comprehensive meta-analysis, also known as an umbrella review, carefully and systematically scrutinized 13 meta-analyses from various databases such as Web of Science, PubMed, Scopus, Embase, and Google Scholar up to January 2023. The new umbrella review that included a total of 77 scientific studies revealed that Q10 supplementation had the following impact on different markers of inflammation and oxidative stress:
- Reduction of CRP (C-reactive protein), which is an inflammation marker and is produced by the liver
- Reduction of TNF-α (Tumor Necrosis Factor Alpha), an inflammation marker that is produced by white blood cells (macrophages/monocytes). TNF-α is also responsible for cell signaling that can trigger apoptosis (programmed self-destruction of cells) and tissue death (necrosis)
- Reduction of IL-6 (interleukin-6), an inflammation marker. IL-6 is released by white blood cells (macrophages) and plays a key role in the acute inflammatory phase and in fever. IL-6 is also produced in fat tissue, which explains why overweight people often have chronic inflammation.
- Reduction of MDA (malondialdehyde), a marker of oxidative stress that follows in the wake of lipid peroxidation, which is essentially a process that rancidifies polyunsaturated fatty acids
- Increases total antioxidant capacity (TAC), which is a measure for the body’s general antioxidant defense
- Increases serum levels of superoxide dismutase (SOD), an antioxidant that neutralizes the free radical called superoxide. SOD plays a key role in the cells’ own antioxidant defense.
The umbrella review also showed that acute Q10 therapy given for a period of less than 10 weeks and in daily doses of 200 mg or higher lowered levels of the inflammation markers, TNF- α and IL-6, and MDA (a marker of oxidative stress.) Also, daily supplementation with 100-200 mg of Q10 for more than 10 weeks resulted in increased antioxidant activity measured by elevated levels of TAC and SOD. The scientists conclude that high-dosed Q10 supplementation may be an ideal add-on therapy for treating chronic inflammation.
What causes chronic inflammation and oxidative stress?
If the immune defense is weak or programmed incorrectly, chronic inflammation may occur. Chronic inflammation increases the risk of oxidative stress, and vice versa. Oxidative stress is when harmful free radicals outnumber the protective antioxidants. Free radicals are generated as a natural byproduct of different metabolic processes in the body. They are also generated by cellular energy metabolism, and the free radical burden increases with age or as a result of an impaired oxygen metabolism. Stress, overweight, smoking, poisoning, medical drugs, heavy metal exposure, and radiation can also increase the number of free radicals and step up the risk of oxidative stress and chronic inflammation.
Why are chronic inflammation and oxidative stress so bad for you?
Both chronic inflammation and oxidative stress are characterized by an overrepresentation of free radicals in the body. What is particularly harmful is when free radicals attack the polyunsaturated fatty acids in the cell membranes (a process called lipid peroxidation) and set off chain reactions in the cells. It is also dangerous when free radicals attack cholesterol, which is otherwise a very important compound. This sets the stage for the formation of atherosclerotic plaque.
High-quality Q10 supplements
A Q10 supplement should ideally be taken with breakfast, as it tends to give a natural energy boost. It is not all that easy for the body to absorb Q10, so make sure to choose a high-quality preparation with documented bioavailability. When taking larger doses in the range of 200-400 mg daily, it is best to take smaller quantities and to let a few hours pass between each dose. That helps the body absorb and utilize the nutrient.
References:
Sara Dabbaghi Varnousfaderani et al. Alleviating effects of coenzyme Q10 supplements on biomarkers of inflammation and oxidative stress: results from an umbrella meta-analysis. Frontiers in Pharmacology 2023
Adrianna Budzinska et al. The bisphosphonates alendronate and zoledronate induce adaptations of aerobic metabolism in permanent human endothelial cells. Scientific Reports 2023
TIP! See also the related articles
Search for more information...
- Created on .








