Rheumatism, aching joints, and inflammation can often be helped with supplements
- and there are no side effects
 Rheumatism is the most widespread chronic disease in Denmark, and many people experience a worsening of the symptoms during the winter period. The majority of people take anti-inflammatory drugs for years, but this increases their risk of bleeding stomach ulcers and other side effects, not to mention premature death. The underlying cause is chronic inflammation and it is a problem that is not properly addressed. For decades, Nobel Prize-winners and other scientists have revealed what causes chronic inflammation and how the problem in many cases can be helped with various supplements that help cure the pain. In the following, we have summarized a lot of the research that has been conducted with vitamin D, fish oil, magnesium, selenium, zinc, and glucosamine, and we have looked at why the anti-inflammatory lifestyle has become such a health trend. It is essential to use supplements that contain the different ingredients in therapeutic doses and with a quality that allows the body to absorb and utilize the active compounds.
Rheumatism is the most widespread chronic disease in Denmark, and many people experience a worsening of the symptoms during the winter period. The majority of people take anti-inflammatory drugs for years, but this increases their risk of bleeding stomach ulcers and other side effects, not to mention premature death. The underlying cause is chronic inflammation and it is a problem that is not properly addressed. For decades, Nobel Prize-winners and other scientists have revealed what causes chronic inflammation and how the problem in many cases can be helped with various supplements that help cure the pain. In the following, we have summarized a lot of the research that has been conducted with vitamin D, fish oil, magnesium, selenium, zinc, and glucosamine, and we have looked at why the anti-inflammatory lifestyle has become such a health trend. It is essential to use supplements that contain the different ingredients in therapeutic doses and with a quality that allows the body to absorb and utilize the active compounds.
When the immune defense protects us humans against infections, poisoning, and cellular damage, it employs a variety of inflammatory processes. However, it is vital for the immune defense not to overreact, as this increases the risk of rheumatism, aching joints, and chronic inflammation that is a common thread in many lifestyle diseases. The unpleasant symptoms are caused by increased blood supply to the local areas and the presence of chemical compounds (cytokines) that are released by the blood cells.
The immune defense, in order to function optimally, needs a variety of different nutrients that support various enzyme processes, antioxidants, and molecular functions. Factors such as lack of sunlight exposure, nutrient-depleted farming soil, poor eating habits, impaired food quality, weight problems, and ageing can deplete our levels of certain very important nutrients that inhibit inflammation. Luckily, this is a problem that we can correct.
Vitamin D and why joint pain is more common in the winter
At our latitudes, the sun during the summer period is our main source of vitamin D. Lack of vitamin D is common due to a variety of factors such as spending too much time indoors, overusing SPF sunscreens, being overweight, being old, and using cholesterol-lowering agents (statins) that block the body’s production of cholesterol (cholesterol is involved in the synthesis of vitamin D). Vitamin D is not just important for bone health. Nearly all the body’s cells have vitamin D receptors, and the white blood cells of the immune system have particularly many. First of all, vitamin D activates our immune defense, which is essential for preventing and fighting infections. Secondly, vitamin D makes sure that the immune system does not “overheat” by controlling and limiting the release of anti-inflammatory cytokines by the white blood cells.
A study from 2016 showed that people with rheumatoid arthritis had lower blood levels of vitamin D and an increased risk of being vitamin D-deficient, compared with healthy controls.
Scientists from National Jewish Health in Denver, USA, have carried out a study, in which they demonstrated that vitamin D’s ability to counter inflammation depends on blood levels of the nutrient. The best results were seen with levels above 50 ng/ml.
The physician can measure your vitamin D levels with a blood sample free of charge. Remember, levels of the nutrient typically decrease over the course of the winter, unless you take a supplement.
Normal vitamin pills for adults (in Denmark) typically only contain 5 micrograms of vitamin D, but this is not enough to inhibit inflammation. There are stronger supplements on the market with 20-80 micrograms. A person’s actual need for the vitamin depends on such factors as sun exposure, age, skin type, BMI, use of cholesterol-lowering drugs, and chronic diseases like rheumatism and diabetes.
Vitamin D is lipid-soluble, which means that we absorb and utilize it best when we take in in capsules where it is bound to oil.
|
Magnesium activates vitamin D and should be balanced correctly with calcium
The form of vitamin D that we synthesize in our skin or take as supplements is an inactive precursor of the vitamin and is named cholecalciferol. Helped by magnesium-containing enzymes, cholecalciferol is converted into its active form in the liver and kidneys. Therefore, if you lack magnesium, it affects your vitamin D status negatively so it is vital to make sure to get enough magnesium from dietary sources and/or from supplements.
Magnesium functions as a gatekeeper in the cell membrane. Here, it makes sure to channel the major part of calcium into the bone cells, while it does the exact opposite by keeping calcium out of the cells in our soft tissues like blood vessels, nerves, connective tissue, muscles, and inner organs. These cells should be kept nearly devoid of calcium in order to function properly.
It is vital to maintain the right balance between magnesium and calcium. If you get too much calcium from dairy products and supplements, or if you lack magnesium, you risk calcium flooding of the cells in your soft tissues. This causes them to overreact so they become stressed and are subject to inflammation.
Did you know that too much calcium at the expense of magnesium may cause muscle cramps and inflammatory conditions?
Nobel Prize-winners discovered the importance of fatty acids
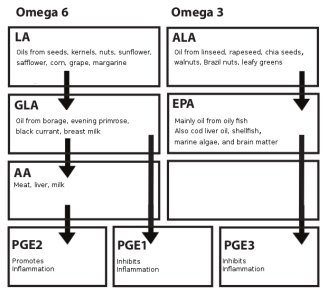
In 1982, the Swedish biochemists, Bergström, Samuelson, and Vane were awarded the Nobel Prize in medicine for their research in some hormone-like compounds called prostaglandins, which are responsible for controlling inflammatory processes in the body.
The different prostaglandins are synthesized from the two essential fatty acids, omega-3 and omega-6. We primarily get our omega-3 from oily fish, while we get most of our omega-6 from vegetable oils. When we ingest these essential fatty acids, they are converted into to the different prostaglandins with help from certain enzymes. Some prostaglandins have pro-inflammatory properties, while others counteract inflammation. It is therefore highly important to maintain the right balance between the different types of prostaglandins. If the balance is disrupted by eating too much omega-6 at the expense of omega-3, chronic inflammation may occur. Since the diet plays such a key role in inflammation, dietary guidelines ought to be issued to those people who suffer from rheumatoid arthritis. It really boils down to pure biochemistry. The following chart gives a rather simple picture of how the omega-6 and omega-3 fatty acids are converted into type PGE1, PGE2, and PGE3 prostaglandins with help from various enzymes.
Simplified overview of the prostaglandin synthesis
|
|
Fish oil, cannabinoids, and therapeutic doses
British researchers analyzed 18 controlled studies, in which patients suffering from rheumatoid arthritis were randomly assigned to therapy with either omega-3 fatty acids or placebo. The conclusion, which was based on the patients’ subjective assessment or a medical evaluation, showed that omega-3 fatty acids have a therapeutic effect on pain. Daily doses between three and six grams of fish oil daily appear to have the best effect. The study was published in 2017 in the science journal Nutrition
Other studies suggest that EPA in particular has the anti-inflammatory effect. It requires daily intake of around 900-1,800 mg of EPA so make sure to read the label so you know how much to take.
According to a study from University of Illinois, where scientists studied animal tissue, omega-3 fatty acids trigger a massive amount of chemical reactions that also lead to the release of cannabinoids (endocannabinoids) with anti-inflammatory properties. According to lead scientist, Professor Aditi Das, the body can release cannabinoids similar to those found in cannabis oil without producing the high that you get from cannabis.
Fish oils based on free fatty acids have the best absorption in the body. Also, make sure to choose a product that is within the official threshold limits for peroxide value and content of environmental toxins.
For the record, it takes around a month before fish oils work optimally. It takes about the same amount of time for the effect to vanish if you discontinue supplementation. Once the symptoms have vanished, you can lower your dose, especially if you use fish oil supplementation in combination with dietary changes.
Oxidative stress and inflammation
Oxidative stress increases your risk of inflammation. Oxidative stress is when the balance between free radicals and protective antioxidants is disrupted. Free radicals are involved in a variety of essential processes, but they must be kept on a tight leash to prevent them from causing cellular damage and inflammation. The free radical burden is increased by stress, overweight, ageing processes, smoking, environmental toxins, microwave radiation, type 2 diabetes, and metabolic syndrome. Our only protection against free radicals is different antioxidant, and selenium and zinc are especially important when it comes to controlling inflammation.
Selenium inhibits inflammation – and farmers have supplemented livestock for decades
Selenium supports around 30 essential selenoproteins, including various enzymes and antioxidants that protect the body against oxidative stress and disease. As mentioned earlier, white blood cells are able to release different cytokines such as interleukin-6 with anti-inflammatory properties. Selenium deficiency is associated with an increased amount of interleukin-6. Also, certain selenium-containing antioxidants (GPx) block interleukin-6 and inflammation. This was observed in a Danish study where selenium supplements stimulated the GPx activity in patients with rheumatoid arthritis. Other studies show that selenium supplementation counteracts aching joints and inflammation by way of several different mechanisms.
Danish farmland is relatively low in selenium and that affects the entire food chain. To compensate for this, farmers have given extra selenium to their livestock for decades to prevent joint inflammation and other diseases that are linked to low selenium levels in the animals.
The reference intake (RI) level in Denmark is 55 micrograms, but many people get far less. In contrast, most studies of selenium involve daily doses of between 100 and 200 micrograms.
Supplements with selenium yeast that provide a variety of different organic selenium species are preferable, as this gives the same natural spectrum that you get from eating a balanced diet with different selenium sources.
There are also supplements that combine organic selenium yeast with organic zinc and other antioxidants.
Did you know that Danish farmland is low in selenium and that farmers have been supplementing their livestock with selenium through decades in order to prevent joint inflammation and other deficiency diseases?
Zinc is important for T helper cells
Zinc is involved in around 1,000 different enzyme processes, many of which are important for the immune defense. A zinc deficiency typically affects the so-called T helper cells, whose job it is to control the immune defense by helping it attack swiftly and withdraw, as soon as the infection is under control or the cellular damage repaired. Zinc is very important for the T helper cells, and therefore a zinc deficiency can weaken the immune defense or cause it to overreact, which can lead to chronic inflammation.
A study from 2014 shows that zinc supplementation inhibits inflammation and oxidative stress in older people. However, many older people have difficulty with absorbing zinc, so even if they appear to be getting enough zinc from their diets, they may in reality be low in the nutrient.
An estimated 25% of the world’s population is zinc-deficient. Severe zinc deficiency is rare in our part of the world, whereas light to moderate deficiency is common. Zinc deficiency and poor utilization of the nutrient may be caused by poor eating habits, too much calcium, alcohol abuse, and diuretics.
Zinc is mainly found in shellfish like oysters, meat, dairy products, nuts, kernels, and beans. Animal sources of zinc are absorbed a lot easier than plant sources. An average Danish diet only provides half as much zinc as the official reference intake (RI) level, which is 10 mg. The European Food Safety Authority (EFSA) has set the safe upper intake level for zinc at 25 mg (for adults).
Glucosamine as medicine against osteoarthritis
Osteoarthritis is a national scourge, for which it takes years to develop. The pain occurs because the articulate cartilage gradually vanishes, causing the exposed bone ends to rub against each other.
Glucosamine is a natural component of joint cartilage, and glucosamine supplements have been used for decades as therapy for osteoarthritis. Glucosamine is normally derived from the shells of crustaceans. According to a report that is issued by the European expert group ESCEO (European Society for the Clinical and Economic Aspects of Osteoarthritis), glucosamine sulfate should be used as first-line therapy against mild to moderate osteoarthritis. The widespread use of painkillers does not help rebuild the cartilage tissue, and this type of medicine is also associated with serious side effects, even death. Science has also found that glucosamine sulfate inhibits the cytokine interleukin-1 that causes inflammation and damages joints.
Glucosamine sulfate is effective for treating and preventing mild to moderate osteoarthritis, where there is still some cartilage left to repair and rebuild. It is important to choose a preparation with pharmaceutical-grade glucosamine sulfate, as this is the form that is documented in studies and has proven to be effective.
Anti-inflammatory lifestyle – the new trend
Inflammation is the common thread in most chronic diseases, including rheumatoid diseases, bowel disorders, diabetes, depression, and cancer. It can hardly surprise that anti-inflammatory living has become the new health trend.
Most importantly, make sure to get all the essential micronutrients you need, as they help counteract inflammation Also, strive to maintain stable blood sugar levels, body weight, and waist circumference, as insulin resistance and excessive body fat (especially visceral fat) sets the stage for inflammation. You can find a variety of recipe books with useful recipes and tips on how to get rid of inflammation.
What supplements to use against rheumatism and joint pain
When attempting to find the right supplements, make sure to give priority to the essential nutrients such as vitamin D, magnesium, selenium, and zinc. Fish oil and glucosamine also play a vital role. Ginger, turmeric, devil’s claw, and rosehip also have anti-inflammatory properties, but it normally requires rather large quantities, and none of the mentioned things are able to replace the essential nutrients.
Did you know that far more lives are lost to prescription drugs than to traffic?Around 730,000 Danes take anti-inflammatory drugs. These products increase the risk of damaged mucosa, poor digestion, bleeding stomach ulcers, heart disease, and blood clots. According to the statistics, prescription drugs cause around 3,300 deaths annually in Denmark. Some of the most dangerous drugs are non-steroidal anti-inflammatory drugs (NSAID) and methotrexate. Just for the sake of comparison, there are over 20 times as many deaths linked to prescription drugs as there are traffic casualties. |
References:
Alan Carter. 8 natural supplements to help fight inflammation. MedicalNewsToday 2019
Manuella Pennisi et al. Vitamin D Serum Levels in Patients with Statin-Induced Musculoskeletal Pain. Disease Markers 2019
William Morrisson. Can vitamin D relieve joint pain? MedicalNewsToday 2019
Aya Mousa et al. Effect of vitamin D supplementation on inflammation: protocol for a systematic review. BMJ Open 2016
National Jewish Health. How vitamin D inhibits inflammation. ScienceDaily 2012
Gerry K. Schwalfenberg and Stephen J. Genuis. The Importance of Magnesium in Clinical Healthcare. Scientifica (Carro) 2017
Anne Marie Uwitonze, Mohammed S Razzaque. Role of magnesium in Vitamin D Activation and Function. The Journal of the American Osteopatic Association. 2018
Forrest H Nielsen. Magnesium deficiency and increased inflammation; current perspectives. J Inflamm Res 2018
Abdulrazaq, Innes JK, Calder PC. Effect of ω-3 polyunsaturated fatty acids on arthritic pain: A systematic review. Nutrition 2017
Lutz Shomburg. Dietary Selenium and Human Health. Nutrients 2017
Hoffmann Peter R et al. The influence of selenium on immune responses. Mol Nutr Food Res.
Kido T et al. Inflammatory response under zinc deficiency is exacerbated by dysfunction of the T- helper type 2 lymphocyte-M2 macrophage pathway. Immunology 2019 Apr.
Ananda S Prasad. Zink in Human Health: Effect of Zink on Immune Cells. Molecular Medicine 2008
MA H et al. Association of habitual glucosamine use with risk of cardiovascular disease: prospective study in UK Biobank. BMJ 2019
Nelson AE et al.: A systematic review of recommendations and guidelines for the management of osteoarthrititis: The Chronic Osteoarthritis Management Initiative of the U.S Bone and Joint initiative. PubMed 2014
https://peoplespress.dk/peter-goetzsche-vi-bruger-alt-for-meget-medicin/
https://pebl.dk/da/nyheder/nyhedsarkiv/fejldosering-med-methotrexat
Search for more information...
- Created on .